Discover new approaches to cardiovascular clinical trials to bring game-changing therapies to patients faster.
















Introduction
Incretin-based anti-obesity medications (AOMs) have proven highly effective in delivering meaningful weight loss, typically 15-25% after one year, which has transformed the management of obesity. However, most people will regain significant amounts of weight after discontinuation of treatment.
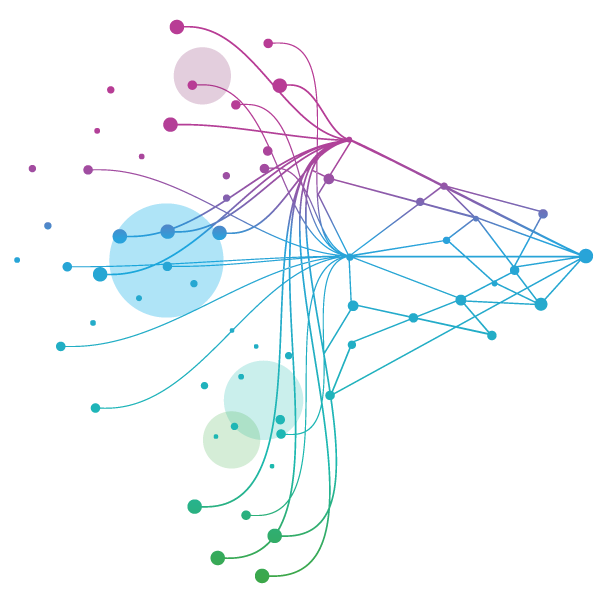
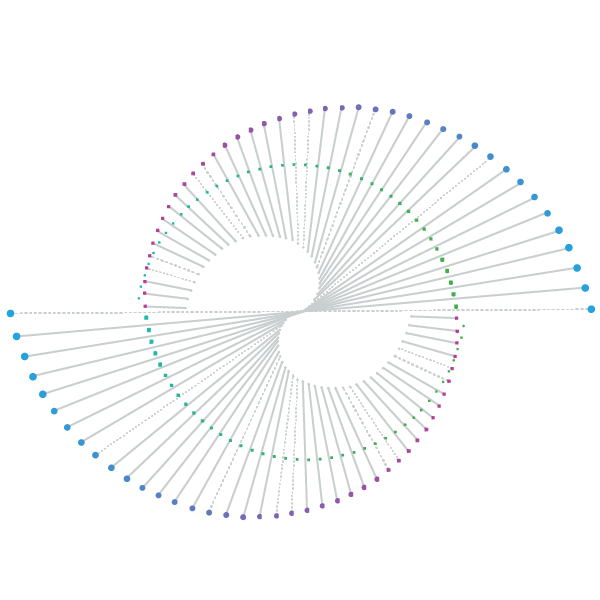
For example, the extension of the STEP 1 phase 3 trial found that patients regained, on average, two-thirds of the weight lost at 1 year after stopping 68-week prior treatment with Wegovy. In the SURMOUNT-4 phase 3 trial, patients switching to placebo after 36 weeks of treatment with Zepbound regained 14% of weight at 1 year post switching, despite ongoing behavioural support, whereas those who continued treatment with Zepbound lost an additional 5% of weight. Furthermore, in both trials improvements in cardiometabolic risk factors that were observed following AOM therapy, such as lower HbA1c, systolic blood pressure or LDL levels, also reversed after AOM treatment was stopped (see Figure 1).

As a growing number of obese or overweight people have now had access to AOMs for a sufficiently long period of time to be able to achieve their weight loss goals, maintaining a healthy weight after initial weight loss will increasingly become a priority.
With the obesity market coming of age, and the focus of AOM therapy expanding beyond induction of weight loss, innovators must understand the different scenarios for how the long-term maintenance of obesity, as a chronic condition, may manifest itself so that they can prepare to seize this opportunity.
The weight maintenance opportunity
Social media conversations about obesity can act as a bellwether for the future direction of this market as patients, and the wider public, share their views on managing obesity and their personal, very real experiences with AOM therapies.
IQVIA’s recent blog [1] on social media conversations in the US and the UK about obesity management revealed some intriguing insight into patients’ intentions once they have reached their weight loss goals:
- 59% of conversations were about continuing on an AOM for weight maintenance, 28% talked about discontinuing treatment for a period of time and then re-starting, while 13% were about stopping treatment altogether once weight loss goals were achieved.
- Of those conversations focused on continuation of AOM treatment, 49% talked about continuing on the same drug, 37% stated continuing on a lower dose, and 14% expressed an intention to switch to a less expensive therapy.
This sentiment not only highlights that weight maintenance is already top of mind for a significant number of patients on AOM therapy, it also points to potential future scenarios that will define the weight maintenance opportunity for innovators and the underlying key drivers – cost, effectiveness, tolerability and convenience.
Key scenarios: How the maintenance opportunity manifests itself
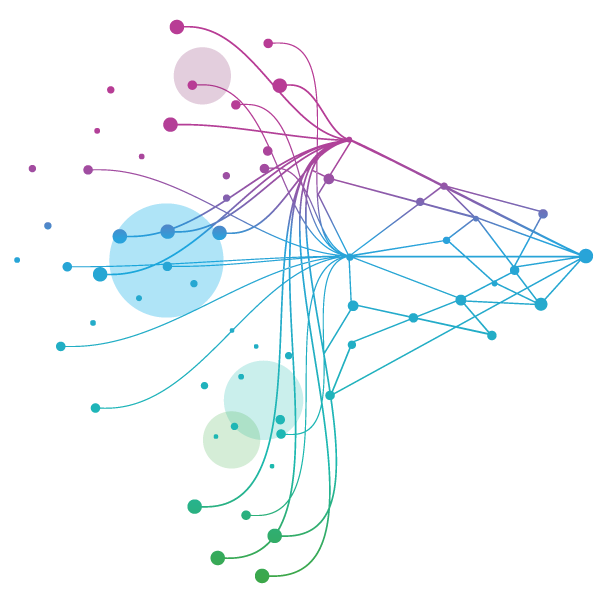
We can identify four macro-scenarios for the maintenance of obesity based on patients’ pharmacotherapy transition following successful weight loss with an AOM induction therapy, including continuation, switching, episodic treatment and discontinuation (see Figure 2).
Lifestyle and behavioural change play a critical role as adjunct to pharmacotherapy during induction of weight loss and arguably even more so in the weight maintenance phase for patients to achieve durable, long-term success. We therefore assume that all weight maintenance scenarios outlined below will include a component of change in lifestyle and behaviour, which, for example, may be facilitated by patient support programmes, including app-based digital tools to promote behavioural change.

1. Continuing with induction AOM: Upon reaching their target weight, patients continue treatment with their induction AOM but may explore a lower dose to modulate effectiveness and tolerability to reflect medical need and patient preference. In future, this situation will apply to both injectable and oral AOMs as potential induction therapies.
In this scenario, patients maintain their target weight over the long term, while benefiting from lasting improvements in cardiometabolic risk factors. Arguably, patients starting on Wegovy have a strong case for continuing treatment after successful induction as it is the only AOM to date with MACE risk reduction included in its label, supported by cardiovascular outcomes data from the SELECT trial, while other, e.g., CNS-related, benefits were observed in real-world studies.
However, this scenario is contingent on a number of prerequisites to achieve the required, high rates of long-term persistence with AOM therapy which contrasts starkly with currently observed real-world persistence levels of 25-30% after 1 year: (i) appropriate pricing of AOMs that ensures long-term affordability in out-of-pocket markets or sustained coverage by payers in reimbursed markets; (ii) adequate long-term effectiveness; (iii) a clean tolerability and safety profile to ensure ongoing treatment without AE-driven discontinuation; and (iv) strong patient motivation, and satisfaction with treatment outcomes, to stay the course.
2. Switching to another AOM: Patients who hit their weight loss target after induction therapy may decide to switch to a different maintenance treatment for reasons such as lower cost, more favourable tolerability or greater convenience.
This scenario will become increasingly relevant as multiple new therapies enter the market over the coming years, thus expanding choice of AOMs for patients, HCPs and payers, where AOMs are reimbursed. For 2026, relevant events include the expected arrival of the first oral therapies, oral semaglutide and oral, small molecule orforglipron, and off-patent semaglutide becoming available in a number of countries, including Canada, India, China, Brazil and Turkey. This will introduce more convenient and lower cost options for maintenance therapy, respectively, and requires us to consider several sub-scenarios:
a. Switch to an injectable, on-patent AOM: To maintain their target weight, patients may switch between the currently approved injectables Wegovy or Zepbound/Mounjaro, or in future to another injectable AOM, as they seek better tolerability and/or lower cost, especially in the case of maintenance therapy at a lower-dose.
b. Switch to an oral, on-patent AOM: Oral AOM therapies have a clear convenience advantage over injectables, which becomes even more pronounced in the context of long-term maintenance therapy. Patients therefore may switch from an injectable induction therapy to an oral AOM for ongoing weight management, provided such therapies offer adequate long-term effectiveness combined with acceptable tolerability.
c. Switch to off-patent semaglutide: Lower cost, off-patent versions of semaglutide may emerge as the maintenance therapy of choice, helping to alleviate the long-term financial burden on patients and health systems from funding ongoing AOM therapy. In reimbursed markets, cash-strapped payers may potentially mandate use of off-patent semaglutide in the maintenance setting.
In these switching scenarios, long-term effectiveness and tolerability, supported by both clinical trials and real-world evidence, alongside pricing will become key determinants of the competitive positioning of different AOMs for weight maintenance.
3. Episodic AOM treatment: In this scenario, patients take a break from anti-obesity pharmacotherapy for a period of time after reaching their weight loss goal, possibly exploring dietary and lifestyle changes instead. Upon regaining weight, patients restart AOM treatment, which could be with either their original AOM induction therapy or an alternative medication, and may involve dose adjustments.
This approach implies weight oscillation over time, with cardiometabolic risk factors most likely sub-optimally managed. Furthermore, the effectiveness of repeated AOM treatment cycles is currently unclear, while posing a potential risk of deteriorating body composition (lean mass vs. fat) due to the cumulative effect of repeated reductions in lean mass. Affordability, restricted access due to time-limited reimbursement which may also be conditional on criteria such as BMI and presence of co-morbidities, and concerns about tolerability and long-term safety of AOMs are likely drivers of this scenario.
4. Discontinuing AOM therapy: Some patients may stop AOM therapy ‘permanently’ once reaching their weight loss goals, with no intention of seeking future treatment, while a subset might actively focus on entrenching dietary and lifestyle changes to maintain their weight. For this group, the importance of continuing with patient support programmes and use of digital tools to promote behaviour change is elevated even further, and it will likely require digital apps to evolve too, to address the specific requirements of this maintenance setting which excludes AOMs.
Ultimately, these patients drop out of the pharmacotherapy-based maintenance opportunity. The drivers of this scenario are similar to those of scenario #3, compounded by a patient mindset that does not consider pharmacotherapy as part of their ongoing weight management efforts.
Understanding these scenarios, and the underlying drivers for how they may play out, is important for innovators to inform their asset strategies, evidence planning and commercial approach to capture the maintenance opportunity.
How innovators should prepare for the maintenance opportunity
As the commercial opportunity expands beyond induction of weight loss to the ongoing management of obesity as a chronic condition, innovators must focus on the following priorities:
- Demonstrating long-term outcomes of their AOM(s), with a particular focus on the maintenance setting. For example, Lilly’s ATTAIN-MAINTAIN phase 3b trial evaluates the efficacy and safety of oral GLP-1 receptor agonist orforglipron for the maintenance of weight in obese and overweight patients who completed the SURMOUNT-5 phase 3b trial, having received tirzepatide or semagutide for 72 weeks. Key endpoints include % maintenance of body weight reduction achieved in SURMOUNT-5 and number of participants maintaining ≥80% of the body weight reduction achieved in SURMOUNT-5, both at 52 weeks, alongside additional secondary endpoints.
In addition to clinical trials, RWE on AOM use in routine practice and their long-term, real-world effectiveness and safety will be needed to substantiate benefits as maintenance therapy. - Elevating tolerability as a strategic differentiator and a key driver of high rates of long-term persistence – a critical success factor for weight maintenance.
For example, Novo Nordisk recently presented data from its REDEFINE 1 phase 3 trial, showing that only 1% of patients taking long-acting amylin analogue cagrilintide over 68 weeks stopped treatment permanently due to nausea. A favourable side effect profile with low discontinuation rates will be critical to position AOMs as suitable long-term treatments. - Strategic pricing that maximises the total commercial opportunity across the induction and maintenance settings. The optimal pricing strategy must be anchored on price elasticity of demand at different stages of the patient journey, tailored to self-pay and reimbursed market segments and reflecting the respective affordability constraints/willingness to pay of patients and payers. Furthermore, there is a role for novel payment models to unlock the maintenance opportunity, e.g., subscriptions, or an outcomes-linked retainer, for example, allowing use of AOMs when weight increases while offering reduced insurance premiums if weight loss is maintained.
- A personalised, patient-centric approach to long-term weight management. This is informed by granular insight to stratify patients into meaningful segments, defined by specific medical needs and personal preferences, with a clear understanding of the drivers of patient choice to guide AOM maintenance therapy positioning as part of a multi-pronged approach including pharmacotherapy, lifestyle, nutrition and behavioural interventions.
- Synergistic co-positioning of different therapies in a multi-asset AOM portfolio. This maximises the portfolio opportunity, and creates differentiation, by seamlessly addressing evolving needs along the patient journey, as patients transition from induction to maintenance, e.g., starting on a high potency injectable followed by an oral maintenance therapy, or use of combination therapies that address more complex patient needs, e.g., multiple co-morbidities or sarcopenic obesity.
Innovators must also keep an eye on novel therapeutic approaches with the potential to disrupt the weight maintenance market, e.g., ultra long-acting injectables that could redefine patient convenience with quarterly dosing, or new modalities such as siRNA therapeutics that have shown promise of durable weight loss in preclinical studies.
The race for the weight maintenance opportunity is on, and innovators must get ready now!
References
- Social Maturity: How have social media conversations about Obesity management and AOMs evolved with the market in two key countries? IQVIA blog, August 2025; https://www.iqvia.com/locations/emea/blogs/2025/07/social-maturity





