Rely on market-leading strategists to help you achieve maximum access and profitability
















- Locations
- United States
- US Blogs
- Disparities in Medicare Access for People Under 65 Living with ALS
Amyotrophic lateral sclerosis (ALS) is a rare, fatal, and progressive neurodegenerative disease characterized by motor neuron loss in the brain and spinal cord. The average age of ALS onset is 55, and people affected experience a progressive loss of motor control, contributing to a median life expectancy of 3-5 years post-symptom onset. While there is currently no cure for ALS, multi-disciplinary care can be employed to help address symptoms, psychological and mobility challenges, and decision-making needs related to ALS. The multi-disciplinary care approach to ALS may include a variety of medications, physical and other therapy, and special equipment that can cost tens of thousands of dollars.
Given the severe nature of the disease, it is essential for people with ALS to have affordable access to care regardless of demographic, economic, or geographic differences. Health equity is one of the top priorities across the healthcare industry. So much so, that the Centers for Medicare & Medicaid Services (CMS) published health equity as the “first pillar” of its 2022 Strategic Plan. As a result, key stakeholders are now actively evaluating ways to ensure that all patients receive the highest quality of care regardless of circumstance. While studies have investigated the relationship between race and ALS diagnosis or mortality rates, little research currently exists regarding accessibility to affordable coverage across the United States and the resulting variations in coverage among individuals with ALS.
Investigating the ALS population and Medigap availability
Recent studies from the National ALS Registry estimate between 5-12 people out of 100,000 in the US may be living with ALS, and IQVIA’s medical claims data observed rates approximate to 15 people diagnosed with ALS per 100,000 captured patients. As the National ALS registry relies on self-reporting, studies have found that it lacks completeness and skews towards capturing more White and younger (less than 65 years of age) patients, and therefore, may not fully represent this population. Accurate measure of the ALS prevalence rates is a key factor in determining National Institute of Health (NIH) funding for ongoing research into the underlying causes and potential treatments of the disease. It is also important for evaluating existing patient access to care. The use of medical claims data, with longitudinal visibility into treatment and coverage, provides further insight into the size of this patient population and can help identify gaps in coverage and care.
ALS prevalence by state (patients diagnosed with ALS per 100,000 people)
(All people identified within LAAD data with ALS in the United States and District of Columbia; 2019; IQVIA LAAD and US census data)
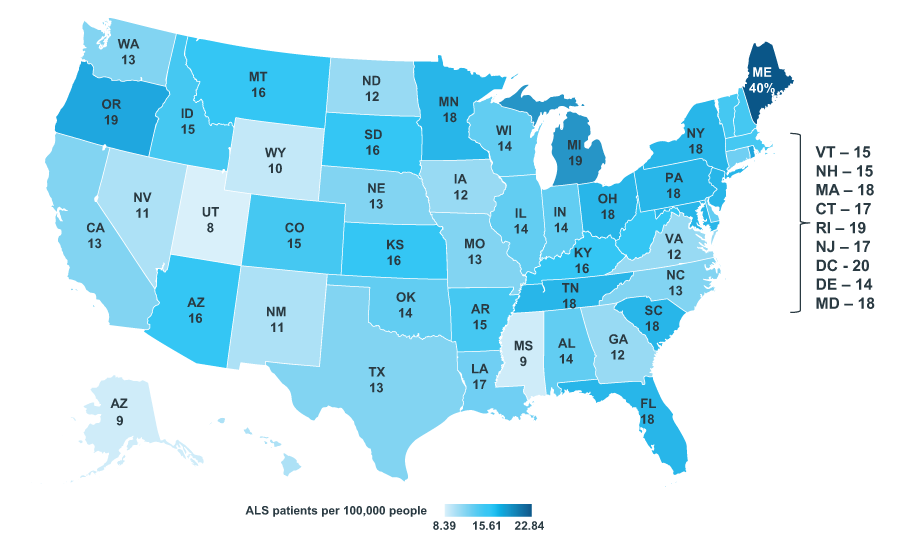
Source: IQVIA 3.0 Data; 2019 US Census Data; US Market Access Strategy Consulting Analysis
Note: The number of patients is associated with all distinct patients active in 2019 within IQVIA’s LAAD dataset with this diagnosis. The state specified for each ALS patient was the state of the provider associated with their first medical claim with a diagnosis code for ALS. Puerto Rico has been excluded due to low sample. IQVIA longitudinal medical claims data captures a subset of the medical claims universe and is representative of patients receiving treatment.
46% of observed people with ALS are under the age of 65. In the U.S., most people under 65 with a disability must wait two years to become eligible for coverage under the Medicare Fee-for-Service (FFS) plan, yet individuals diagnosed with ALS, regardless of age, are eligible to begin receiving Medicare benefits immediately under federal law. The accelerated Medicare eligibility is intended to provide a safety net for this (under 65) segment of the ALS population so that they can maintain coverage for treatment and care. Without the current Medicare policy, people under the age of 65 would remain exclusively dependent on private insurance or Medicaid for coverage. The prevalence of people with ALS under 65 varies by state, with South Carolina representing the highest proportion of patients under 65, and Wyoming and Idaho the lowest.
Proportion of total people with ALS under 65 by state
(All people with ALS present in data from January 2019 - June 2021)
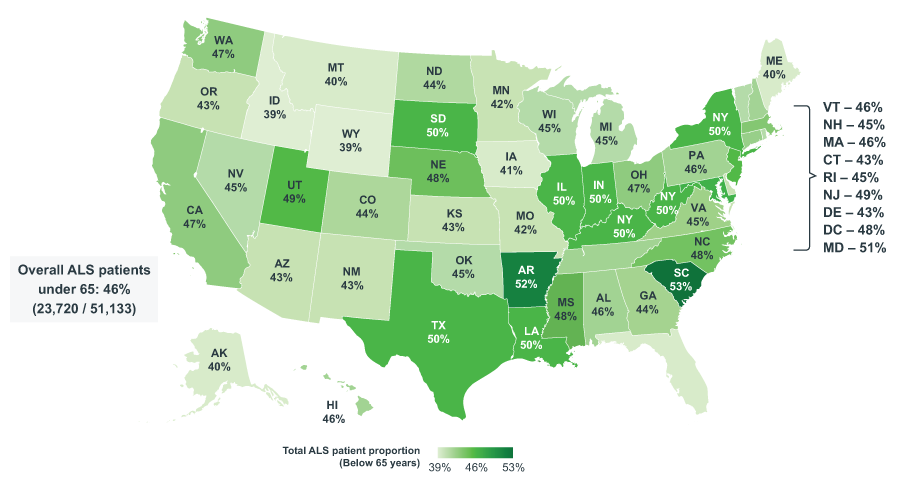
Source: IQVIA 3.0 Data; US Market Access Strategy Consulting Analysis
Note: The number of patients is associated with all distinct patients active in 2019-2021 within IQVIA’s LAAD dataset with this diagnosis. The state specified for each ALS patient was the state of the provider associated with their first medical claim with a diagnosis code for ALS. Puerto Rico has been excluded due to low sample.
Regardless of the type of healthcare coverage an ALS patient may have – private, Medicare FFS, or Medicaid – additional barriers like patient cost-sharing may still prevent patients from obtaining treatment. An average patient with Medicare FFS typically spends more than $5,000 in out-of-pocket costs throughout the course of a year; patient claims research as of 2019 showed that Medicare FFS patients with ALS (without supplemental Medigap coverage) may pay over $36,000 a year depending on stage of disease and their access to affordable coverage.
For people diagnosed with ALS who are enrolled in Medicare FFS, supplemental coverage in the form of Medigap insurance is a vital option – though its availability varies state-to-state. Medigap coverage can reduce a patient’s out-of-pocket costs to as little as $0 annually for medical treatment, leaving patients only needing to pay monthly premiums. Currently, there is no federal policy that requires access to Medigap insurance for beneficiaries under 65. There are some states, including Oklahoma and Maine, that require insurers to offer coverage to beneficiaries under the age of 65. Other states, such as Ohio and Nevada, do not require any Medigap plans to be offered to beneficiaries under age 65.
Only 17 states, representing 43% of people under the age of 65 diagnosed with ALS, require Medigap coverage for all Medicare beneficiaries at rates equivalent to patients who are 65 or older. In these states, this access to Medigap coverage provides a significant benefit to this under-65 patient population by lowering their costs for medications, therapy, and other healthcare-related services. By providing equitable coverage options for people with ALS, regardless of age, these states help ensure comprehensive access to affordable care and treatment.
An additional 39% of people under 65 with ALS receive their healthcare in states where Medigap plan options must be available to all Medicare patients, but this access comes with some caveats. Some of these states (11) allow higher premiums among those eligible under 65 years old, which may render coverage unaffordable even if it is available. Other states (5) offer Medigap coverage but with fewer plans available than what is traditionally offered to those over 65. Finally, 18% of people with ALS live in states that do not currently require that Medigap be available for Medicare patients under the age of 65. Patients in these states have the highest potential for exposure to prohibitive cost burdens for medications and other healthcare related treatments and services. While half of these people (9%) do not reside in states that have guaranteed issue rights (i.e., an insurance company can choose not to sell these patients a Medigap policy), some states (12) do have payers that offer Medigap voluntarily.
In lieu of Medigap coverage, people with ALS may also seek to enroll in alternative healthcare plan options, if available and eligible, to attain more affordable coverage. For example, these patients may use coverage provided by the Department of Veteran’s Affairs (VA) or seek third-party foundational support. Those that qualify as dual-eligible for Medicaid and Medicare are also able to reduce their Medicare benefit costs. While these options can be effective in reducing patient costs for those who qualify, the VA, third-party foundations, and dual eligibility are not available to all patients and could further be supplemented by greater access to Medigap in all states.
ALS Medigap coverage for Medicare patients under 65 by state
(All people with ALS under 65 years of age; January 2019 – June 2021)
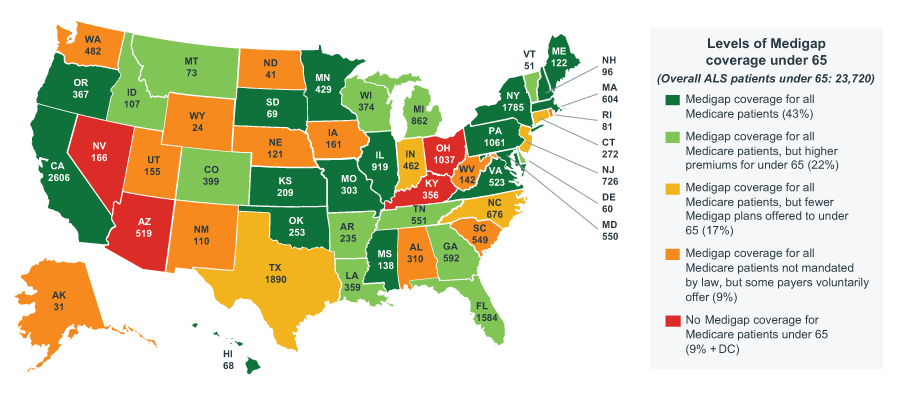
Source: HealthInsurance.org as of 2021; IQVIA LAAD 3.0 Data; US Market Access Strategy Consulting Analysis
Note: The number of patients is associated with all distinct patients active in 2019-2021 within IQVIA’s LAAD dataset with an ALS diagnosis. The state specified for each ALS patient was the state of the provider associated with their first medical claim with a diagnosis code for ALS.
Discussion
For all people with ALS to have access to quality care, gaps in affordability must be addressed. For many patients with ALS who are under the age of 65, enrollment in Medicare can provide much-needed coverage, however, for this group of individuals, the coverage may still come with prohibitive out-of-pocket costs that can delay access to therapy or other types of care. The opportunity to supplement Medicare FFS coverage with Medigap is not universal, nor is it guaranteed, creating inequities in access and therefore treatment.
Depending on the underlying demographic characteristics of people within each state – consider the geographic variation in race, wealth, etc. - a lack of uniformity in Medigap policy may impact the coverage options available to underserved or underprivileged individuals with ALS. Though important, Medigap availability is only one access challenge, and the investigation of patients’ barriers to treatment is necessary for people with ALS and beyond. IQVIA is committed to leveraging its data and market insights to further support and improve the delivery of affordable, high-quality, equitable care for people with ALS in collaboration with industry, patient, provider, payer, and other stakeholders across the U.S. healthcare market.
Acknowledgements
The authors would like to thank several IQVIA colleagues for their support and contributions. This includes but is not limited to Luke Greenwalt, Conrad Bhamani, Sayf Al-Omaishi, Sally Little, and Nita Akoh. The authors would also like to acknowledge Biogen for sponsoring the analyses used in this blog. The findings and final editorial decisions belong to IQVIA.

Patient Affordability and Engagement Services
Increasing patient access to your brand requires engaging and educating eligible patients and health care professionals on the details of your therapy as well as removing the burden of cost from the patient.
Related solutions
Increase patient access and adherence.
Gain high value access and increase the profitability of your brands
Data, AI, and expertise empower Commercial Solutions to optimize strategy, accelerate market access, and maximize brand performance.




