





















- Blogs
- The Opioid Crisis the data the science and the humanity
I had the privilege of participating in a panel discussion at BIO 2019: Opioids: Changing the paradigm of treating pain and addiction - one year later, which examined how far the issue has evolved since 2018’s BIO sessions.
The discussion was a landmark experience, reminding me of the human impact of data, science and research. Human Data Science isn’t just about numbers and methodology, it’s about improving human health and bringing science to support decisions sometimes colored by bias and stigma.
There are few untouched by the tragedy of opioid abuse. It has devastated families and the societal cost is evident in the urban, suburban and rural communities in which we live. Unlike other diseases, opioid abuse often carries a societal stigma and a raft of judgments that make it even more difficult to address the problem. Our biases can even spill over into the clinical setting, where people from certain racial and ethnic backgrounds are less likely to be prescribed pain medication and more likely to be suspected of drug-seeking behavior.1,2
All of us who study and deliver health care - and set the policy and standards of care that inform treatment for opioid abuse - are struggling. Our focus at the IQVIA Institute is to help optimize human health by bringing data and fact-based insights forward to better inform decision makers in this critical area.
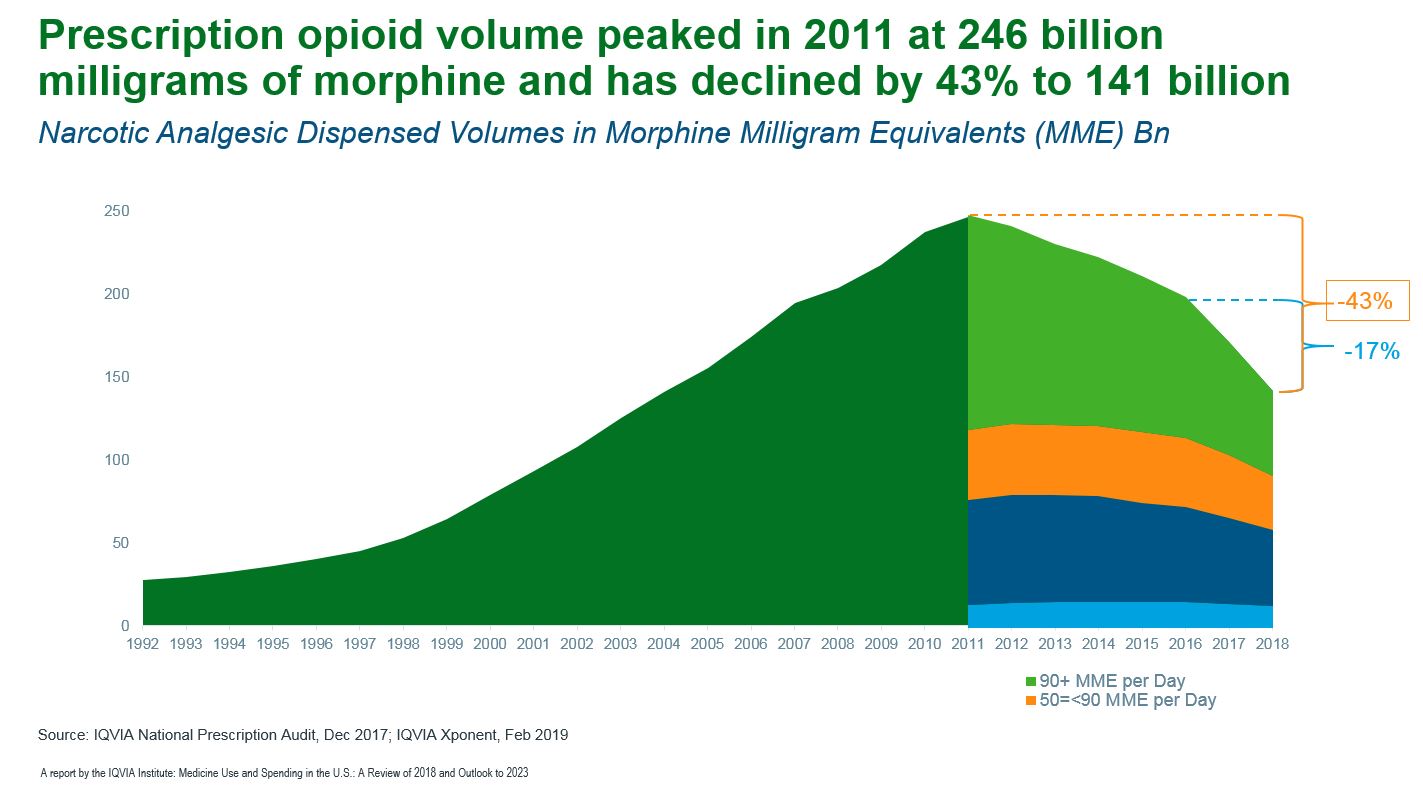
In our recent study, Medicine Use and Spending in the U.S. - A Review of 2018 and Outlook to 2023, we reviewed, among other topics, the trends and effectiveness of our opioid strategies. Prescription opioid volume continued to decline steeply last year as changes in regulations and clinical guidelines, accompanied by high public awareness, drove a 17% decline in total morphine milligram equivalents (MME) dispensed. The biggest decline came from the most potent and dangerous high-dose prescriptions. Prescription opioid volume has declined 43% since the peak in 2011, with prescriptions for 90 MMEs per day or greater declining by 61% (see exhibit).
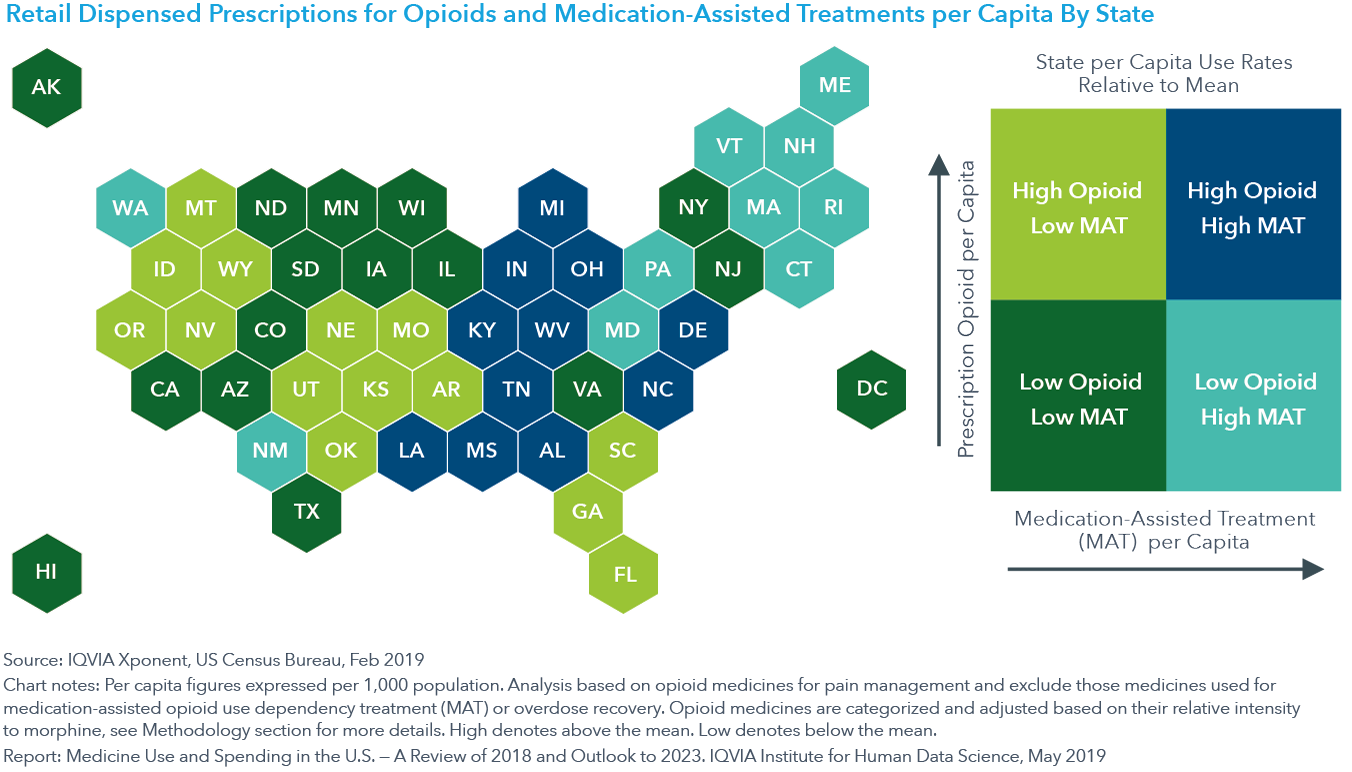
But as the U.S. experiments with different state- and local-level policies to address regional concerns, the progress has been uneven. States still differ significantly in their per capita use of opioids and medication-assisted treatments (MATs) for substance abuse disorders. All the New England states have enacted new controls on opioid prescribing and support for opioid dependency in the past three years, but they already had lower-than-average opioids per capita but higher MATs per capita. Other states, including those hardest-hit by the opioid crisis, experience relatively high per capita use of both opioids and MATs (see exhibit).
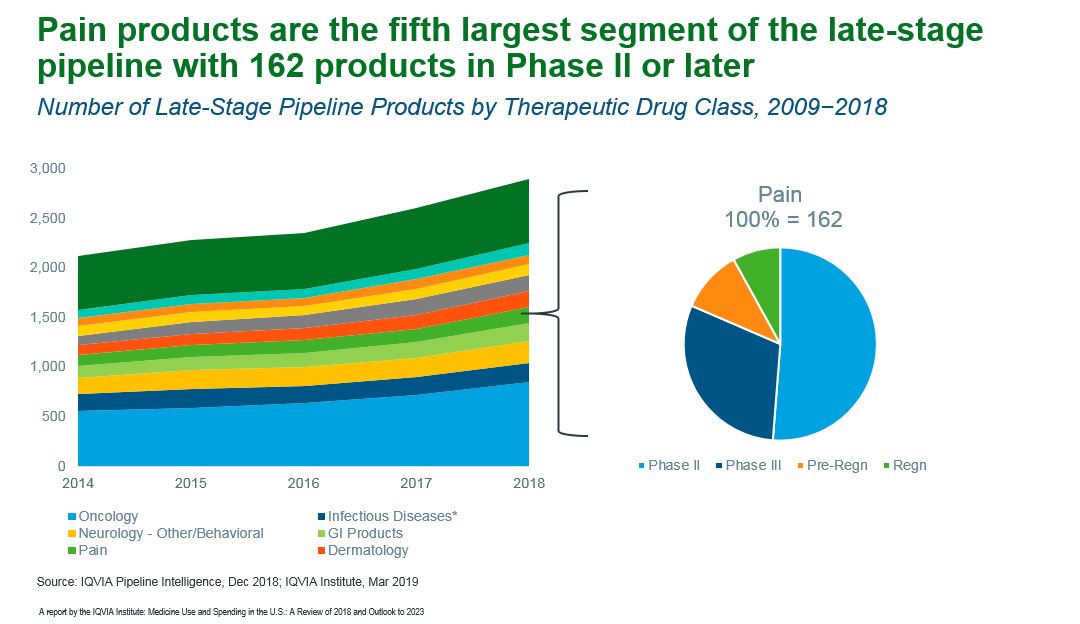
Of course, we’re not really addressing the opioid crisis if we create another crisis by taking pain treatment away from those who have no other options. Pain medicines, including non-narcotic drugs, declined by 21 million prescriptions, driven significantly by the declines in prescription opioid use with little, if any, offsetting use of other types of pain treatment. To address the unmet need, pharma companies are researching medicines and devices that are effective and less addictive, with pain products representing the fifth-largest segment of the late-stage pipeline (see exhibit).
How do we reduce the suffering of every human experiencing pain, while minimizing the equally painful impact of addiction? There are no easy answers, but the available data could illuminate a path forward for practitioners, researchers and policymakers.
First, there must be an awareness that judgments and preconceptions have been shown to cloud perceptions and influence decisions, preventing us from most effectively addressing all aspects of pain treatment and the opioid crisis.
Second, in the battle against opioid abuse, it is important to remember that improving the health and well-being of humans applies equally to those with severe and intractable pain. Through the intelligent, individualized application of improved standards of care and the development of alternative pain-management approaches, there is the potential to reduce the public-health crisis while addressing the individual crisis of the person in pain.
And importantly, better decisions can emerge by continually tracking the effectiveness of the standard-of-care and policy experiments in different states and countries.
It is our hope that the work of the IQVIA Institute for Human Data Science can continue to make valuable contributions in these efforts.
1 Singhal A, Tien YY, Hsia RY. Racial-Ethnic Disparities in Opioid Prescriptions at Emergency Department Visits for Conditions Commonly Associated with Prescription Drug Abuse. PLoS One. 2016;11(8):e0159224. Published 2016 Aug 8. doi:10.1371/journal.pone.0159224
2 Fischer MA, McKinlay JB, Katz JN, et al. Physician assessments of drug seeking behavior: A mixed methods study. PLoS One. 2017;12(6):e0178690. Published 2017 Jun 23. doi:10.1371/journal.pone.0178690








