





















- Blogs
- Understanding Patient Behavior for Improved Experience and Better Results
Understanding Patient Behavior
Patient behavior plays a crucial role in adherence and the success of the treatment. Healthcare Professionals (HCPs) who understand patient behavior and behavioral models and frameworks can design more successful patient support programs that are aware of the needs of their patients. Knowing the physical and psychological strains of a patient’s illness and his/her behavioral response also allows HCPs to empathize and better communicate with them.
Pharmaceutical companies can also benefit from understanding patient behavior. It helps them design and structure treatments in ways that improve patient self-management and adherence and provide a better patient and caregiver experience. Pharmaceutical companies can also help patients improve their medication adherence and self-management, leading to better results and reduced burden on the healthcare system. This, in turn, will also improve payer and HCP’s perception of the brand.
Patient Behavior Models
The Biopsychosocial Model
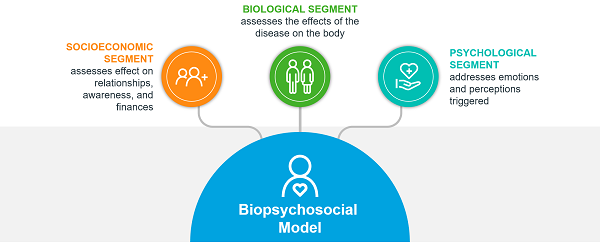
Several models have been designed to help approach patient behavior and explain it. One such model, the biopsychosocial (BPS) model, considers three attributes that impact the patient’s body and surroundings: the biological, psychological, and socioeconomic conditions.
- The biological segment of the model assesses the effects of the disease on the body. This includes:
- The affect of symptoms on daily life
- The fluctuation of the symptoms and the resulting feeling of uncertainty
- The need for surgical interventions that are not cures in advanced stages of a disease
- The psychological segment addresses the emotions and perceptions triggered by the presence and symptoms of the disease. This includes:
- Increased anxiety and depression among patients
- The perception that the lack of self-management and stress are causes, and the resulting feelings of guilt or anger
- The socioeconomic impact of the disease assesses how it affects the patient’s relationships with friends and family, the patient’s awareness, and his/her financial situation. This includes:
- The need or preference to avoid social situations when the condition creates problems or uncertainty (e.g. uncertainty with bowel movements)
- Perceived stigma and increasing sense of isolation
- Fatigue and pain restricting social interactions, leading to further isolation
- Financial burden affecting access to needed treatment
The Biopsychosocial Model
The BPS model allows for a holistic approach to patient support to help reduce the disease burden on the patient. It helps categorize the patient’s ‘lived experience’. The information gathered through the model provides HCPs with a complete understanding of the patient and allows them to improve patient’s overall treatment experience.
BPS Model: The Five Core BeliefsThe BPS model looks at five core belief categories to tackle and enhance patient adherence:
- Identity: The abstract label of the disease, along with the symptoms associated with the condition, are addressed. These are explained clearly to the patient in a manner that he/she can fully grasp.
- Cause: In several cases, patients may feel that the perceived cause (e.g. stress) is manageable without treatment. In other cases, the patient may feel an emotional burden or guilt if he/she feels at fault for the condition. That is why the actual root cause of the condition is also explained to emphasize the importance of the treatment.
- Consequences: Clarifying the impact of the condition and the treatment are also crucial in ensuring and maintaining adherence. If the perceived impact is too little, it may dissuade patients from implementing required changes, and if the impacts are major, it may make it difficult for them to prioritize.
- Timeline: Another important belief category that needs to be addressed, based on the BPS model, is the treatment timeline. Ensuring the patient fully understands the complete treatment timeline is critical in avoiding early discontinuation.
- Cure/Control: A patient’s perceived lack of control over his/her condition may discourage him/her from undertaking required self-management behaviors. Clarifying a patient’s impact on his/her own health and condition may help eliminate or reduce that perception.
Another model that helps explain patient behavior and the elements that influence it is the Capability-Opportunity-Motivation Behavior (COM-B) framework. COM-B is a theoretical framework that helps explain and identify the barriers to and facilitators of behavior. It divides behavioral drivers into three categories: capability, opportunity, and motivation. While all three categories directly influence behavior, capability and opportunity can also indirectly impact behavior through their effect on motivation.
Capability-Opportunity-Motivation Behavior (COM-B) Framework
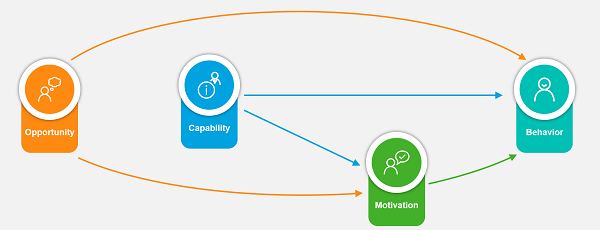
- Capability describes the patient’s physical and psychological capacity to engage in a specific behavior. This also addresses the patient’s capacity to perform the necessary physical and thought processes needed for successful treatment.
- Motivation discusses the brain processes that energize and direct behavior. This includes reflective processes (evaluating and planning) and automatic processes (emotions and impulses arising from associative learning and/or innate dispositions.
- Opportunity addresses all the factors lying outside the individual that prompt certain behavior or make it possible. Opportunities can be both physical (e.g. access to healthcare and HCP-patient communication) or social (e.g. social stigma toward disease or religious or cultural beliefs).
Converting Patient Behavior Insights into Actions
Effective patient support goes beyond providing patients with important treatment information. It utilizes proven behavior change techniques to improve patient engagement and adherence in the long term. To do so, it is essential to understand what drives behaviors, what activates behavioral barriers in each patient, how those barriers can be removed, and what facilitates behavioral changes.
There is a dichotomy between research on patient behavior, with some focusing on factors that drive adherence and others focusing on ways to change behavior. One approach that works on bridging the gap between these two is the Behavior Change Wheel.
With the Behavior Change Wheel approach, the COM-b model is used to categorize and conceptualize factors that explain or determine individual health-related behaviors, including the mechanisms between the factors. This gives us a starting point to map effective Behavior Change Techniques (BCTs) and interventions, enabling us to better use these insights to design patient support. Evidence-based BCTs, guided by psychological theory, target the determinants that shape behavior. There are currently 93 BCTs described by taxonomy that can help change behavior.
Case in Focus: Patient Behavior in Action
Patient behavior was assessed to propose new measures to design better patient support programs for improved patient adherence in Phenylketonuria (PKU).
PKU is an inborn error of metabolism that results in high levels of the amino acid phenylalanine (Phe) in the blood and may lead to permanent neurological impairment, intellectual disability, seizures, delayed development, and mental and psychosocial disorders as early as infancy and childhood. Proper treatment can prevent neurocognitive impairment and improve the quality of life if the care plan is managed properly and if the caregiver and patient are adherent.
The analysis of patient behavior looked at the treatment process and the barriers and drivers in the following phases: Testing initiation, Trial initiation, Treatment initiation and management, and Transitions and adjustments.
Patient behavior was analyzed using the COM-B framework to identify the barriers and drivers to patient adherence and find solutions. Several barriers were identified:
- Health literacy and numeracy challenges
- Insufficient information about the treatment
- Perceived cost or access issues
- Assumptions that current dietary efforts are enough
- Lack of physician psychosocial support
- The treatment’s complexity and side effects.
Several drivers for patient behavior change were also identified, including:
- The ability to increase dietary protein
- Feeling better since starting treatment
- The inability of diet alone to keep phenylalanine (Phe) concentration under control
Upon completion of the study, several recommendations were made to improve patient uptake and adherence to the PKU treatment, including:
- Employing a multichannel approach to aid learning and retention
- Addressing multiple stages in the patient journey from engagement to ongoing treatment
- Providing skills training on health literacy/numeracy and the impact of high Phe levels
- Providing information about treatment efficacy and safety profile
- Offering tools to drive effective treatment and dietary self-management
- Offering nutrition advice alongside psychological and behavioral strategies to manage concerns
- Offering emotional support tailored to patients’ and caregivers’ needs
- Facilitating peer-to-peer education and support
A proper understanding of patient behavior and applying that understanding can lead to reliable patient adherence and, subsequently, effective and successful treatment. Through patient behavior models and frameworks, such as the biopsychosocial model and the COM-B framework, appropriate enhancements can be made to the treatment plan to encourage better adhere. Pharmaceuticals can design improved treatment systems that better cater to patients’ needs and allow for enhanced self-management of treatment.





