















- Blogs
- We've Got Your Back! An Innovative Study Combining Digital Patient Generated Data with Health Records
New data sources, technology, and study methods are providing additional opportunities to traditional research approaches. From recruitment through to data collection, novel methods are accelerating research timelines, increasing data quality, and reducing burden on both participants and physicians.
The UK-based We’ve Got Your Back Study effectively demonstrates the opportunities of a novel approach. This observational, multi-center cohort study captured patients’ symptoms and experience of acute and chronic back pain leveraging an innovative, enriched methods approach.
Data-driven site selection
Study sites were carefully selected based on the type of software system available and the number of potentially eligible patients. By excluding 40% of sites within the National Institute for Health Research (NIHR) Clinical Research Network (CRN) based on network intelligence including non-research-active sites, low number of eligible patients, and absence of Egton Medical Information Systems Limited (EMIS Health), the electronic medical record (EMR) software, the study team could focus on maximizing enrollment efforts on the remaining 60% of sites. As a result, among sites initiated in the study, 88% invited patients to join the study, and 73% of sites successfully consented participants.
Seamless recruitment and connected data
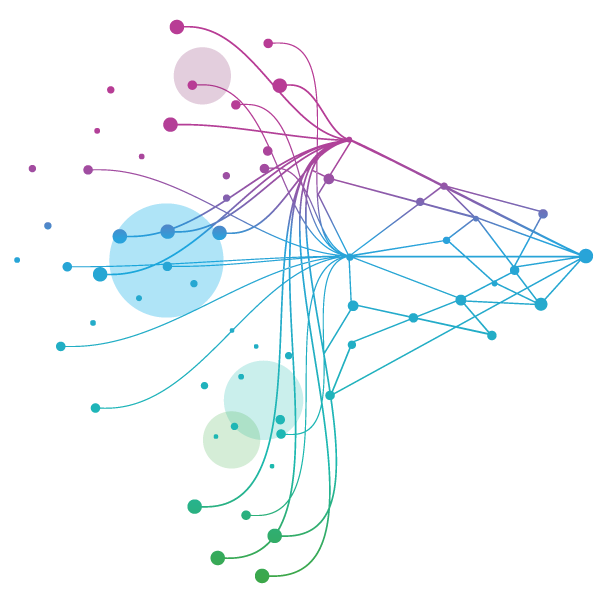
Reducing participant burden and establishing strong connections between real world patient reported data and EMR data were study priorities. Patient recruitment and data connections progressed through the following:
Eligible patients were identified and flagged automatically to physicians through the EMIS EMR system based on specific characteristics, eliminating the need for physicians to remember each study inclusion criteria.
Physicians discussed the study with their patient, and if interested, patients would provide a verbal consent to receive more study information and a link to download the uMotif study app via text or email.
---------------------------------------------------------------------------------------------------------At this point, a unique patient ID was generated and recorded in the patients’ EMR. The text or email sent to the patient also included this unique ID. The unique ID was critical for linking the EMR data and the patient generated app data at an individual patient level while allowing the final study data to remain anonymous.
---------------------------------------------------------------------------------------------------------
The patient downloaded the uMotif app, was asked to enter their unique ID, and consented to take part in the study. The study description and consent, including information on how their data would remain anonymous, was also available to participants in the app to review.
At the end of the study, IQVIA will access the EMR data and the patient generated app data to build a combined dataset. The anonymized data will then be analysed in line with the primary and secondary objectives.
Through this approach, 60% of the total number of study participants had been enrolled by the fourth month of recruitment.
Easy-to-use technology for patients
For patients, the uMotif app provided the added benefit of being able to more effectively manage their condition by recording symptoms and tracking trends or exacerbations. For the study, collecting direct, real-time patient generated data was critical to eliminating recall bias, generating reliable real world data, and had the potential to reduce costs and the time to collect. Out of the 322 patients invited, 42% downloaded the app, consented to enrol, and provided regular data.
In 2019 Pfaff, E., Lee, A., Bradford, R. et al1 published results from the pragmatic trial ADAPTABLE. The study compared different recruitment methods in the identification of patients taking different daily doses of aspirin. Study results proved the efficacy of electronic methods to recruit patients and reach a wider study population. For the We’ve Got Your Back Study the consent rate through electronic recruitment was 11% higher than that of the ADAPTABLE study.
Burden-reducing approaches for physicians
With increasing demands on general practitioners’ time, the study focused on ways to reduce physician burden, both during initial recruitment and ongoing data collection. Beyond automatically flagging eligible patients, the study significantly reduced the need for primary data collection by leveraging secondary data. More than one third (42%) of data variables required for the study were collected from EMR data, greatly reducing the risk of transcription errors e.g. when copying data from health records to CRFs, and relieving administrative burden for physicians and research delivery teams.
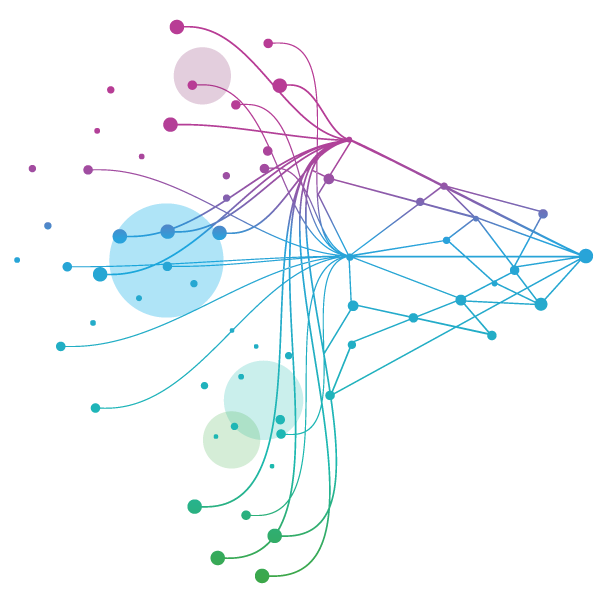
At the end of the study, participating physicians were surveyed to better understand how the study methods impacted their participation and willingness to recommend a similar approach to others.
We’ve Got Your Back End of Study Physician Questionnaire, 2019
The We’ve Got Your Back Study is a step forward in the way we utilise technology and digital methods to identify, recruit, and engage patients to obtain real-time data. A user-friendly app in the hands of patients reduced burden and bias while capturing timely data. By leveraging an enriched methods approach through secondary data, the study streamlined the information needed from both physicians and patients, simplifying participation for both and generating insights for a better understanding of back pain.
The study is being delivered in partnership with:- National Institute for Health Research (NIHR) Clinical Research Network (CRN) who supports research within the NHS, and are hosted by the University of Leeds, the Sponsor of the study.
- uMotif Limited, the data capture platform on which the app was built.
- IQVIA, a clinical research organization, who managed the study from protocol development through to analysis and provided the software service, which supports health care professionals to ‘prescribe’ digital health content such as mobile phone apps to patients.
- Egton Medical Information Systems Limited (EMIS Health), the electronic medical record (EMR) system provider to GP practices.
1. Pfaff, E.; Lee, A.; Bradford, R. et al. Recruiting for a pragmatic trial using the electronic health record and patient portal: successes and lessons learned. JAMIA 0(0), 2018, 1–6.











