IQVIA Vigilance Collect is a web and mobile app for receiving adverse events, allowing patients, HCPs, pharmacies, patient support programs and medical representatives to report adverse events in a user-friendly way.
















- Blogs
- Case Study: Solving the Adverse Event Communication Bottlenecks with Vigilance Collect
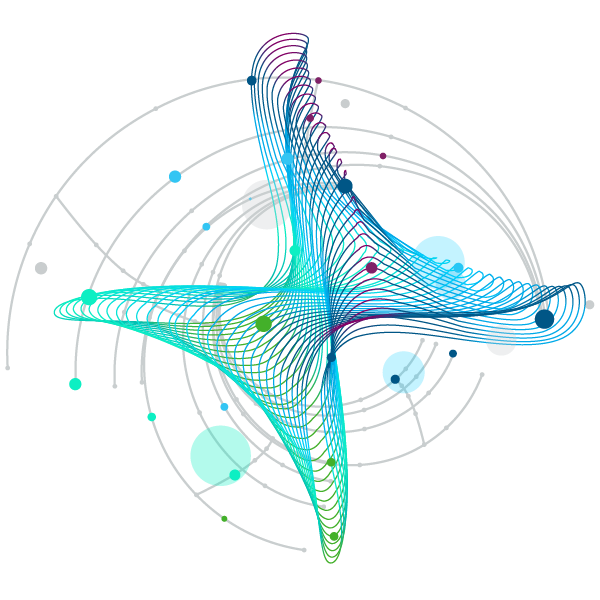
Digital transformation is empowering leaders to rethink many of their legacy processes that can be more streamlined and intuitive to drive better outcomes. As the combination of data collection and processing technologies in life sciences has picked-up pace, pharmacovigilance has been a prime functional area to see benefit almost immediately.
Adverse event (AE) collection is one such function that has significant bearing on the ability of a life sciences company to protect patients and maintain compliance after marketing approval. However, the legacy processes for AE collection are not fast or agile enough to accomplish this effectively. One of the top ten global pharmaceutical companies first recognized this challenge in 2012 and partnered with Foresight, an IQVIA company, for consultation around how to collect AE data closer to or directly from the source to best capture the accurate, relevant data behind the AE report.
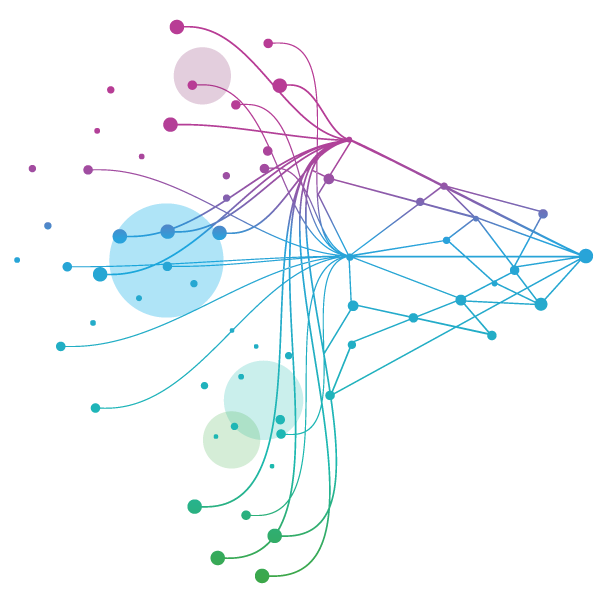
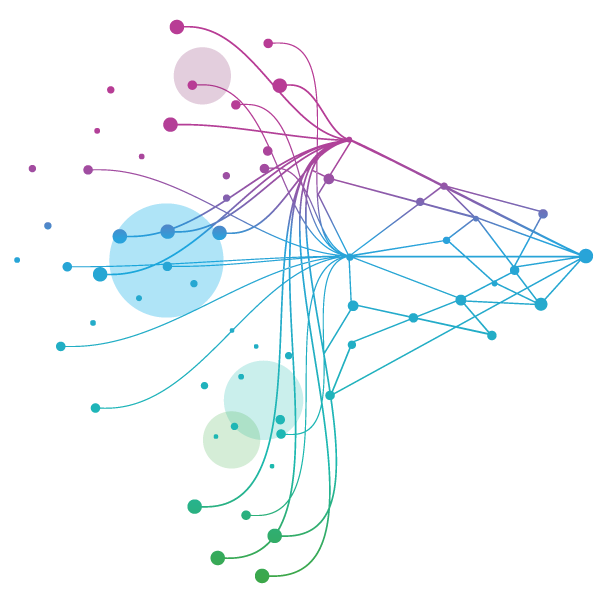
Today, that company is processing more than 120,000 cases a year (>15% of intake) with IQVIA Vigilance Collect, a module of the IQVIA Vigilance Platform that leverages web and mobile portals for the capture and follow-up of AEs directly from the reporter or person suffering the AE. This technology adoption has been the underpinning for substantial cost savings and superior pharmacovigilance management and outcomes. However, to understand the significance of its impact, we must first understand the historical methods behind of these processes.
How Adverse Events Are Traditionally Collected
In the most common scenario, an AE concern is collected through the following steps:
- A patient describes an AE during a medical consultation.
- Their doctor relays it to an administrative assistant, who transcribes and sends it via email to the product manufacturer’s in-country patient safety mailbox, which may be managed by a third party.
- Once the email is translated as needed, sometimes by another third party, the data is extracted and transferred onto a standard AE form.
- It will then be sent to a central processing group (usually another third party and off shored) for processing, where it is entered into a global drug safety system.
- The entered data will often be reviewed by another person for accuracy.
- The case is reviewed by a safety medic; this is probably the first person looking at the case with an understanding of the significance of the event to the safety profile of the drug.
By the time a case makes it to a person qualified to make a judgement call, the case data has potentially transformed five to six times by different people. This clunky process can easily become the catalyst for poor judgement based on distorted information. Furthermore, the initial report can spur follow-up questions from those with a deeper knowledge of the risk profile of a product. Should those questions arise, the question must travel back through the process. By the time these questions make it back to the doctor who saw the patient, it has been several days, and it is unlikely they have an answer. Though regulations stipulate that the organization follow up a minimum of two times for a response, companies report follow up success rates between 1-2% from their outgoing enquiries.
Thus, companies are often spending time and money on disparate third-party providers that do not communicate with one another, as well as on administrative tasks performed by internal experts to vet the information and make sense of it. Even so, cost is far from the biggest driver to rethink the approach.
According to Dr David Lewis, visiting Senior Visiting Research Fellow in Pharmacovigilance at the University of Hertfordshire, safety remains the number one priority. “As the Qualified Person Responsible for Pharmacovigilance (QPPV), it was critical that we found a means of capturing original source data to improve the reliability of our evidence. The combination of technology and partnership with IQVIA enabled our team to do exactly that.”
The life sciences industry is rapidly understanding that they must be driven by the experiences of the patients they effect, and that safety is a core component of those events. The more patient reported AEs are transformed, the further out of reach patient centricity becomes. Closing the gap between the data source and the final analysis of an AE is essential to achieving true patient centricity in life sciences.
A Better Path Forward with Technology
In this case of the global pharmaceutical company, Vigilance Collect allowed it to put the power of AE reporting directly into the hands of people and patients. Either individually or together with their health providers, the application enabled direct input into the global safety system from a computer or mobile device. This mitigated the intermediate transformation of the information, including most translation requirements as the platform is equipped to auto-translate seven different languages.
By removing the degrees of separation between the pharmacovigilance team and the data source, Vigilance Collect additionally enabled a 100% response rate to follow-up questions. Drug/Event combinations are programmed into the system so that the reporter gets asked the relevant risk management questions at the point of contact. As a result, the company was able to draw out specific information about AEs, and in turn, implemented more proactive safety measures.
With Vigilance Collect, the company reduced its case processing costs by 30-40% as the case processing partner provided a discounted price for pre-entered cases (in E2B format). Case collection systems remain relatively uncommon to date, as they are not mandated by the regulators, and they incur additional costs. However, as these cases are significantly easier to process and minimize the need for multiple third parties, the return on the initial investment can be quickly realized.
Most importantly, digital transformation in pharmacovigilance enabled by these types of tools trigger a fundamental shift in the industry on the accuracy of qualitative data. “The generation of high-quality datasets can prompt medical safety specialists to focus on the details of AEs that may have otherwise been lost in translation or during coding,” Lewis says. “Those companies that leverage tools and technology to expand the scope of their pharmacovigilance case intake will position themselves as the true champions of patient centric practices as the future of safety surveillance unfolds.”
For more information, please visit the IQVIA vigilance page. For additional questions, please send an email to safetypv@iqvia.com.
Related solutions
IQVIA Vigilance Platform is our secure SaaS environment built to simplify safety and PV processes, while boosting speed, accuracy, and efficiency.
Discover how AI and ML reduce risk and increase efficiency in adverse event reporting
Vigilance Case provides real-time management, oversight and reporting of Safety cases, streamlining operations by automating low value activities.
Multi source signal detection and management





